Senior Sask. doc fears 'unthinkable' decisions about who gets care during 4th wave 'not far off'
'We are 1 major multi-vehicle car crash or major trauma away from an unheard-of turning point': Dr. Susan Shaw
Saskatchewan may be bringing back mandatory masks and introducing a proof-of-vaccination program for non-essential businesses to help blunt the fourth wave of COVID-19, but those in charge say difficult decisions may still lie ahead for the province's health care workers.
Scott Livingstone, the CEO of the Saskatchewan Heath Authority (SHA) — the operational arm of the province's health system — said in a news conference Thursday that COVID-19 patients admitted to hospital today are people who were infected two weeks ago.
"There's very little we can do today to stop [those future hospital admissions] from happening, other than building capacity, supporting our staff and using tools like slowdowns," Livingstone said of steps already announced late last week.
Saskatchewan had 218 COVID-19 patients in hospital as of Thursday, including 48 people in intensive care units. The province hasn't seen that many infected people in ICUs since the third wave, when there were 49 infected ICU patients on April 25. And those figures do not even include ICU patients without COVID-19.
During a virtual town hall with physicians on Thursday night, the SHA signalled that it had moved to the second of four escalating phases of ICU capacity, compared to the first stage three weeks ago.

In the first stage, coded green, the system has enough beds for those who need to be placed in ICUs. Saskatchewan works with a base of 79 ICU beds, distributed throughout the following communities:
- Battlefords Union Hospital (North Battleford): 3.
- Victoria Hospital (Prince Albert): 8.
- Royal University Hospital (Saskatoon): 15.
- St. Paul's Hospital (Saskatoon): 12.
- Regina General Hospital Surgical ICU: 10.
- Regina General Hospital Medical ICU: 10.
- Pasqua Hospital (Regina): 7.
- Cypress Regional Hospital (Swift Current): 4.
- Five Hills Health Region (Moose Jaw): 4.
- Yorkton Regional Centre: 6.
In the second stage, coded yellow, the system is challenged and health care is affected; hence the service slowdowns (including elective surgeries) announced late last week, which allow the province to "surge" to up to 116 ICU beds by redeploying staff.
The SHA directed its workers last week to surge even further, to up to 130 ICU beds, including 80 ICU beds for COVID-19 patients.
In a table shared among SHA division heads before Thursday's town hall — a document which was obtained by CBC News — projections were shared indicating that Saskatchewan could see a rolling seven-day average of 125 infected people in ICUs by Sept. 30.

"We will use all resources available to us to care for both COVID and non-COVID patients during this time," Livingstone said during the news conference of the coming weeks.
"But we will be tested as an organization like we have never been tested before."
'An unheard-of turning point'
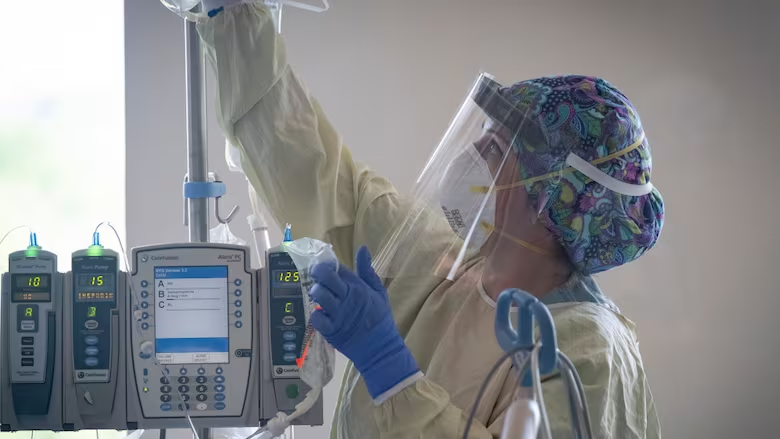
Dr. Susan Shaw, the SHA's chief medical officer, said she feared the health system is edging closer to having to make "unthinkable" decisions about who gets care and who does not, under the SHA's "Saskatchewan Critical Care Resource Allocation Framework."
The ethical framework has been in place since the beginning of the COVID-19 pandemic and is used on a case-by-case basis, Shaw said.
"We are already deciding which patient's surgery will be delayed to create space for COVID patients and who needs to be transferred to another facility because we need their bed for sicker COVID patients."
But Shaw said she's worried the framework will need to be put to more use in the coming weeks.
"That this is the case when we have a vaccine, when we know what other measures can prevent and control COVID-19, breaks my heart," Shaw said in a Thursday note to health care workers obtained by CBC News.

Shaw said the system is one major multi-vehicle crash or major trauma away from "an unheard-of turning point."
"I am worried we are not far off from having to make decisions about who receives life-saving care, and who receives palliative care, who gets ICU care, and who does not. Our resources are being stretched thin."
Health care workers need Saskatchewan citizens to get vaccinated, stay masked and keep their distance from each other, she said.
Dr. Saqib Shahab, Saskatchewan's chief medical health officer — who makes public health recommendations to the Saskatchewan government — echoed Shaw during the news conference. He said much depends on what people do or don't do in the coming weeks.
"We are reaching a phase where if things continue unabated, people who have COVID won't have an ICU bed. People who don't have COVID but have a heart attack won't have an ICU bed. And of course, people who are waiting for urgent surgery will keep getting delayed. So I think things are at a critical juncture."
Dr. Alex Wong, an infectious disease physician with the SHA, said the new measures announced Thursday are "a good start."
Masking will be required in all indoor public spaces beginning on Friday.
On Oct. 1, people visiting a wide range of non-essential businesses — from movie theatres to nightclubs — will be required to show proof of full vaccination or proof that they recently tested negative for COVID-19 (at their own cost, according to Premier Scott Moe).
"I'm not super confident that this is going to be enough," Wong said, adding that he's hopeful Saskatchewan will follow Alberta's lead and also limit the size of gatherings again.
"When you look at our curve relative to Alberta's curve, we're on that same super dangerous, steep upward trajectory," he said.

Dr. Shahab said that if hospitalization numbers don't decline, "as we've said before, other measures will have to be on the table."
However, it's the Saskatchewan government that ultimately decides whether to act on Dr. Shahab's recommendations.
Moe, when asked Thursday if he took responsibility for the fourth wave of COVID-19 in Saskatchewan, said his government is always making decisions "collaboratively" and with "the information that we have at that point in time."
with files from Sam Maciag and Leisha Grebinski
